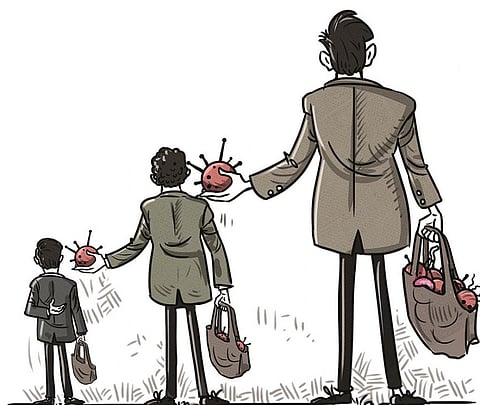
Grab the pathogens, but don’t share the drugs
Illustration: Yogendra Anand / CSE
At the Geneva headquarters of the World Health Organization (WHO), complicated negotiations are going on to reach consensus on a Pandemic Access and Benefit Sharing (PABS) system. This is central to a new international treaty on pandemic prevention, preparedness and response that WHO hopes to finalise by May this year for the approval of its 194 member-countries.
To many readers, the question of sharing pathogens might seem esoteric. Why is there a need for a PABS system to access pathogens—these are in the main viruses and bacteria along with fungi, protozoa and worms—and to share the benefits from their utilisation? After all, for more than half a century, formal and informal networks have existed for sharing pathogens and influenza viruses have been exchanged freely through WHO.
This is because the landscape was altered by two UN agreements, the Convention on Biological Diversity (CBD) and its supplementary pact, the Nagoya Protocol, which came into force in 1993 and 2014, respectively, and sought to make PABS a vital component of fighting disease. While CBD agreements gave nations sovereign rights over their genetic resources including microorganisms, these did not make access or benefit sharing any easier. For one, they did not guarantee timely access. Delays or refusals for pathogen-sharing have resulted in sub-optimal vaccine composition and diagnostics that were not tailored or tested against the original or new variants of pathogens, according to experts. And missing completely from the picture was any kind of benefit sharing.
The most dramatic example of this remains the case of Indonesia, which in 2007 refused to share H5N1 influenza virus samples after an outbreak of avian flu in the country. The genomic sequence data of H5N1 as with any virus, were needed to track the virus's evolution, develop vaccines and diagnostics and also to monitor drug resistance. While Indonesia has been pilloried for its decision in January 2007 to stop sending H5N1 viruses to WHO’s reference labs, much of the blame lies elsewhere, not least with the apex health organisation itself. Indonesia had followed protocol at the start of the problem.
It identified the first human H5N1 cases in July 2005 and sent clinical specimens to two labs in WHO’s influenza surveillance network, that is, the US Centers for Disease Control and Prevention (CDC) and Hong Kong University, for confirmation and risk assessment till the end of 2006. In the meantime, scientists started reporting results of analyses of H5N1 viruses without first notifying or getting permission from Indonesia as the rules demanded. Articles were published in scientific journals without including Indonesian experts at a time when a cluster of cases in the country signalled an impending pandemic. This contravened the WHO guidance issued in March 2005 concerning the timely sharing of viruses with pandemic potential. At the time, Indonesia was on edge having reported 81 human cases along with the highest fatality rate of 63 deaths.
Because of fears of a pandemic, Indonesia was also criticised for releasing genetic data only to a small network of research bodies linked to WHO and CDC although that was all it was required to do.
It then decided that all its H5N1 virus sequence data should be deposited in GenBank while it continued to send samples to CDC for risk assessment and generation of seed viruses for vaccine production. In spite of following the protocol it got nothing in return. The final straw was confirmation of reports that an Australian company planned to develop an H5N1 vaccine from a virus that Indonesia had provided to WHO. This “was not only in violation (again) of the WHO guidance for virus sharing (March 2005) but also . . . revealed the unfairness and inequities of the global system,” as Indonesian scientists pointed out in a 2008 article in a scientific journal.
In its defence, Indonesia argued that pathogen samples given freely by developing countries are used by companies in rich nations to develop vaccines and other products that are unaffordable in the donor countries. Indonesia justifiably sought a guarantee that it would benefit from products derived from the isolates it was sharing.
This experience of being short-changed has been a recurring theme at WHO negotiations on PABS. In the first of the meetings held by WHO in 2007 to resolve the virus-sharing issue, Thailand was blunt.
Its representative to WHO’s executive board meeting was quoted thus: “We are sending our virus [samples] to the rich countries to produce antivirals and vaccines. And when the pandemic occurs, they survive and we die. . . . We are not opposed to the sharing of information and virus [samples], but on the condition that every country will have equal opportunity to get access to vaccine and antivirals if such a pandemic occurs.” But no solution has been found yet to address the breakdown of trust in the global flu surveillance system. A major change was signalled in the early days of the COVID-19 pandemic when China shared on a public database the first genetic sequence data (GSD) of the virus which causes the novel coronavirus disease. The GSD was shared within a couple of weeks of the first cluster of the severe acute respiratory syndrome-coronavirus-2 or SARS-COV-2 being reported (see “Sharing pathogens but not the benefits during pandemics”, Down To Earth, February 1-15, 2021). The GSD was shared with WHO and GenBank, a partnership of the US, Europe and Japan.
However, the underlying problems persist. At the current round, the eighth meeting of WHO’s Intergovernmental Negotiating Body (INB) which ended on March 1, the schism between rich countries and the developing world seemed as wide as ever, with many blaming the WHO secretariat for failing to facilitate impartial negotiations. Over 70 countries from two groups, the Africa Group (48 countries) and Group for Equity (29 countries), have proposed comprehensive text proposals for the PABS system to provide legal and financial certainty, effectiveness and accountability, both in sharing access to pathogens and GSD.
Top among the proposals made in February was the setting up of a WHO-coordinated laboratory network, PABS database and legal devices like Standard Material Transfer Agreements. Ethiopia made it clear what the African member-states want: a multilateral PABS with clear data governance and accountability for sharing pathogens and a “dedicated financing mechanism with inclusive governance”.
Intellectual property (IP) is a major sticking point. Developing countries have sought a safeguard that no IP is allowed on “WHO PABS biological material, including its GSD, or parts thereof, in any form including any modified form or for any use”. That is a tough nut to crack since scientists from the developed north have always patented data extracted from developing countries without the knowledge of the latter. Can these humps be crossed? The next meeting of INB is on March 18, making the time for convergence extremely short as the pandemic treaty deadline looms closer.
This was first published in the 16-31 March, 2024 print edition of Down To Earth