International Women's Day: Empower to protect the womb and newborn
On International Women’s Day, I sieved through the mounting data on the impact of dirty air on maternal health and children.
A lot has been written about the toxic effects of killer air on the elderly, children, women and poor. But what is going on inside the womb that locks in ill-health in the new generation and kills mothers? How do we understand this health evidence to empower and propel action?
We have not yet attached primacy to the fact that most of the illness and deaths that occur among mothers and children because of mothers’ exposure to toxic air are avoidable and modifiable. A generation can be saved if we act on time. Health impacts of exposure to air pollution during the prenatal period cannot be overlooked in health policy.
It is well-known that invisible, killer air is a leading cause of deaths and illness in India. Nearly all Indians are breathing air pollution levels that exceed the World Health Organization's Air Quality Guideline. Reports of the World Health Organization (WHO) and a large number of health journal articles have warned us about the ill-effects of air pollution during pregnancy and embryonic phases of development. Are we responding to these evidences?
The evidence
Scientists tell us that the foetus is extremely sensitive and vulnerable to oxidative stress during pregnancy that can have long-term impact early and later in life. If air pollution affects a mother’s respiratory health, the delivery oxygen and nutrients to the foetus can be reduced.
Maternal exposure to air pollution can increase the risk of development of airway disease in offspring due to impaired lung development in utero. Particulate matter can stimulate maternal inflammatory responses, reduce maternal immunity and increase the risk of infection. Adverse birth outcomes include preterm birth or stillbirths and poor neurodevelopment.
Evidences put together by the WHO shows that placental damage, epigenetic changes and maternal inflammatory responses can influence birth weight. Many studies from Guatemala, India, Pakistan and Zimbabwe show higher risks of low birth weight due to maternal exposure to smoke from stoves using solid fuels and increases the risk of low birth weight by 38 per cent.
In India, Kalpana Balakrishnan and her team have, for the first time, investigated the link between exposure to PM2.5 during pregnancy and low birth weight in an integrated rural–urban, mother–child cohort in Tamil Nadu. They have followed a cohort of 1,285 women in the first trimester of pregnancy in primary health care centres and followed them until the birth of their child to collect data on maternal health, prenatal care, exposure to air pollution during pregnancy and the birth-weight of the child.
They have found that a 10 μg/cum increase in exposure to PM2.5 during pregnancy can decrease birth weight by 4 gm and lead to a 2 per cent increase in the prevalence of low birth weight after adjustment for other factors. They have also compared the outcomes between households using clean fuels and solid fuels and found that a 70 gm decrease in birth weight was associated with solid fuel use.
Scientists studying foetal physiology say that exposures during early pregnancy — when there is high oxygen demand and rapid cellular changes — may cause structural or genetic damage. According to a study published in Journal of Midwifery & Women's Health, pregnancy induces significant maternal physiological changes over a short period of time and these changes increase a woman's risk when exposed to pollutants.
This also increases foetal exposure because many pollutants pass through the placenta. Due to increased ventilation rate, pregnant women inhale more pollutants than non-pregnant women and this increases the risk of lung damage.
More studies have linked outdoor and household air pollution with hypertension in pregnancy that kills many mothers and leads to preterm birth or low birth weight and leads to health complications later in life, including endocrine, nutritional, and metabolic diseases.
Studies have also linked maternal exposure to nitrogen oxide and sulphur dioxide in the months before pregnancy to increased risk for gestational diabetes mellitus. In fact, overall paternal exposure before conception (mother and father) can lead to lower birth weight.
A cohort study conducted in Wuhan, China, found a significant association between maternal exposure to atmospheric PM2.5 during early pregnancy and congenital heart defects in the offspring. Another extensive study on maternal exposure to ambient air pollution in Bangladesh has found a strong link between ambient air pollution and child stunting.
These irrefutable evidences must provoke strong action.
Empower to act
Gender- and child-sensitive air pollution control measures need urgent attention. Even when such policies are in place, economic and social barriers weaken their quick uptake.
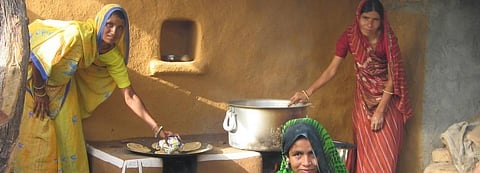
For instance, the ongoing programme of providing subsidised clean cooking fuel LPG — Ujjwala — to poorer households has expanded substantially and yet not to the desired level. While some households are still too poor to use even the subsidised fuel on a sustained basis, there are also social blocks.
Households are not fully aware of the effect of their daily cooking habits on their own health and children. Their investment in clean cooking fuels is not often a priority. It is necessary to build household-level awareness. Also, clean fuel policy will have to be even more refined further to make clean fuels accessible and affordable for all.
But this is not an action agenda only for the poor households. Toxic risks have grown for all income classes. Exposure levels will have to be cut drastically for the rich and the poor across all neighbourhoods and regions. Calibrate action immediately for measurable deep cuts in all forms of exposure from cooking, vehicles, industry, power plants, burning of waste and toxic dust. This is non-negotiable.
Health and air pollution science must empower and inform change for all. Transmission of latent risk from toxic air through wombs is not acceptable.